Table of Contents
- Introduction………………………………………………………………………………………………………….. 1
- Clinical features and epidemiology…………………………………………………………………………… 2
- Diagnosis……………………………………………………………………………………………………………… 5
- Disease management……………………………………………………………………………………………… 7
- Vaccination…………………………………………………………………………………………………………… 9
- References………………………………………………………………………………………………………….. 10
These guidelines for the clinical management of lumpy skin disease (LSD) are an integral part of the National Guidelines for Lumpy Skin Disease Control in Bangladesh. This document provides basic information on the history, economic importance, clinical manifestations and diagnosis of the disease, and suggestions for the management of LSD cases.
The procedures that this document sets out for the diagnosis and clinical management of LSD are based on the recommendations of the OIE Terrestrial Animal Health Code1 and the OIE Manual of Diagnostic Tests and Vaccines for Terrestrial Animals2, FAO Field Manual on Lumpy Skin Disease3, as well as local veterinary field experiences in Bangladesh. The readers are encouraged to consult these documents for further detailed information.
This document was developed by the Department of Livestock Services (DLS) with Technical Assistance Services (TAS) from the Food and Agricultural Organization of United Nations (FAO, UN). The targeted audiences of these guidelines are the field veterinarians actively involved in the detection and clinical management of LSD cases in Bangladesh.
1. Introduction
Lumpy skin disease (LSD) is an acute to chronic, highly infectious and economically important trans-boundary animal disease of cattle and water buffalo, characterized by fever and generalized nodular lesions on the skin. The disease is caused by a poxvirus closely related to sheep pox and goat pox viruses, which belong to the genus Capripoxvirus under the family Poxviridae. The virus is primarily transmitted by biting insects.
1.1. History and distribution
The disease was reported for the first time in Southern Africa, in Zambia, in 1929 and then became endemic across Africa and the Middle East. Since 2015, the disease has spread into the Balkans, the Caucasus and the southern Russian Federation.
As of November 2020, the introduction of the LSD virus was confirmed in several countries of South Asia, including Bangladesh (July 2019), China and India (August 2019), Nepal (June 2020), Taiwan (July 2020), Bhutan and Vietnam (October 2020), and Hong Kong (November 2020)1.
1.2. Economic importance
Outbreaks of LSD cause substantial economic losses in affected countries, but while all stakeholders in the cattle industry suffer income losses, poor, small-scale, and backyard farmers are hit hardest. The disease impacts heavily on cattle production, milk yields, and animal body condition. It causes damage to hides, abortion, and infertility. Costs of veterinary service and treatment add to direct losses. Indirect losses stem from restrictions on cattle movements and trade.
1.3. LSD in Bangladesh
The first outbreak of LSD in Bangladesh was detected on 22 July 2019. Cases were identified in three upazilas (Anowara, Karnofuli, and Patia) in Chattogram district of Chattogram division. Although the origin of the LSD virus in Bangladesh remains unresolved, the first affected areas were located in the usual in-bound trade routes of cattle arriving in Bangladesh through formal and informal transboundary animal movement from neighboring countries.
1 Roche, X., Rozstalnyy, A., TagoPacheco, D., Pittiglio, C., Kamata, A., Beltran Alcrudo, D., Bisht, K., Karki, S., Kayamori, J., Larfaoui, F., Raizman, E., VonDobschuetz, S., Dhingra, M.S. and Sumption, K. 2020. Introduction and spread of lumpy skin disease in South, East and Southeast Asia: Qualitative risk assessment and management. FAO animal production and health, Paper 183. Rome, FAO. https://doi.org/10.4060/cb1892en
2. Clinical features and epidemiology
2.1. Susceptible species
LSD mainly affects cattle, although water buffalo can be affected. Exotic cattle (Bos taurus) and cross-bred cattle are generally more susceptible than the indigenous zebu cattle (Bos indicus). LSD has been observed in wild ruminants but is not transmissible to humans.
2.2. Incubation Period
The incubation period in experimentally infected animals varies between 4 to 7 days, but in naturally infected animals it is usually 4-14 days and can extend up to 5 weeks. According to the OIE Terrestrial Animal Health Code1, the incubation period is considered to be 28 days for regulatory purposes.
2.3. Clinical signs
LSD signs range from inapparent to severe. The following clinical signs may be observed:3
- High fever (>40.5 °C) which may persist for approximately a week
- Lacrimation and nasal discharge – usually observed first
- Subscapular and pre-femoral (superficial) lymph nodes become enlarged and are easily palpable
- A sharp drop in milk yield
- The appearance of highly characteristic, nodular skin lesions (Figure 1) of 10-50 mm in diameter:
- The number of nodules varies from a few in mild cases to multiple in severely infected animals
- Predilection sites are the skin of the head, neck, perineum, genitalia, udder and limbs
- Deep nodules involve all layers of the skin, subcutaneous tissue and sometimes even the underlying muscles
- Necrotic plaques in the mucous membranes of the oral and nasal cavities cause purulent or mucopurulent nasal discharge and excessive salivation, containing high concentrations of virus
- Typically, the center of the lesion ulcerates and a scab forms on top
- Skin nodules may persist for several months
- Sometimes, painful ulcerative lesions develop in the cornea of one or both eyes, leading to blindness in the worst cases
- Skin lesions in the legs and on top of the joints may lead to deep subcutaneous infections complicated by secondary bacterial infections, myiasis and lameness
Some long-term complications have been observed:
- Pneumonia caused by the virus itself or due to secondary bacterial infections
- Mastitis
- Permanent or temporary infertility in bulls
- Abortion or anestrus lasting for several months
In a postmortem examination, pox lesions can be found throughout the entire digestive and upper respiratory tracts and lungs, and on the surface of almost any internal organ.

Figure 1: Characteristic skin nodules (disseminated cutaneous papules with necrotic centers) in LSD affected cattle
2.4. Morbidity and mortality
- Morbidity is variable depending on the course of the disease outbreak and the immunity status of the herd. About 10-20% of animals can be affected at the onset of an outbreak. Morbidity can reach up to 40% in calves aged < 1 month.
- A cumulative mortality rate of 1-5% is considered usual. An investigation conducted by the Epidemiology Unit of DLS, Bangladesh reported 2.7% mortality.
2.5. Transmission
- LSD is primarily a vector-borne disease. Biting insects such as the common stable fly (Stomoxys calcitrans), the mosquito (Aedes aegypti) (Figure 2), and some tick species of the Rhipicephalus and Amblyomma spp., have demonstrated the ability to spread the LSD virus.
- Short-distance transmission is dependent on how far the insects fly to change hosts between feeds. However, movements of cattle may allow the virus to jump over long distances (Figure 3). Direct contact is considered ineffective as a source of infection but may occur in some cases. Infected animals showing lesions in the skin and mucous membranes of the mouth and nasal cavities excrete infectious LSD virus in saliva, as well as in nasal and ocular discharges,
which may contaminate shared feeding and drinking sites. Infectious LSD virus has been detected in saliva and nasal discharge for up to 18 days post-infection.
- The infectious virus remains well-protected inside crusts, particularly when these drop off from the skin lesions. The farm environments may remain contaminated for a long time in the absence of thorough cleaning and disinfection practices. Newly introduced cattle to the LSD virus contaminated holdings may become infected with the virus persisting either in vectors, the environment, or both. Intra- or inter-herd transmission may also occur via contaminated needles during vaccination or other injections if needles are not changed between animals or herds.
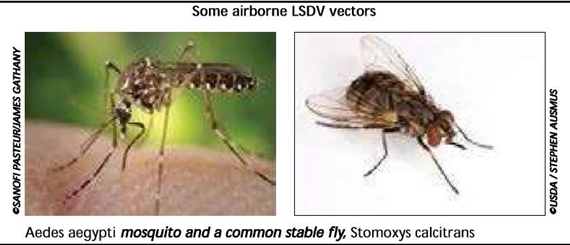
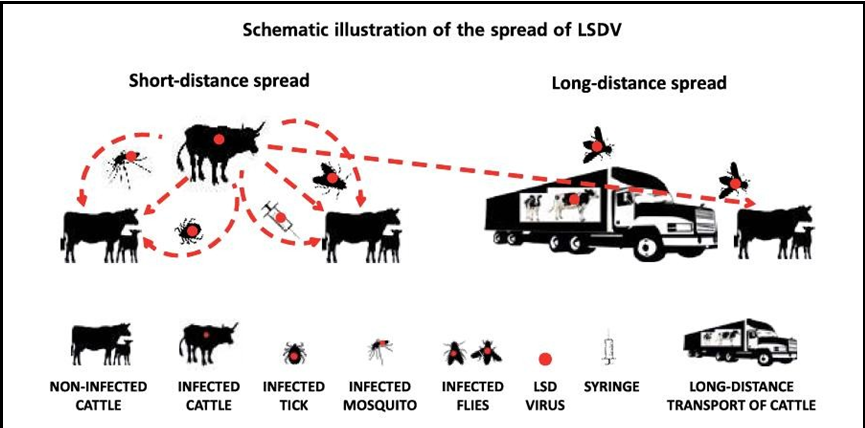
Figure 3. Short-distance and long-distance transmission of LSD virus3
- LSD virus can be transmitted through nasal secretion, saliva, milk, semen, necrotic tissue, and vaginal secretion
- Contaminated fomites, clothes, equipment, feeders and waterers, syringes and needles (including artificial insemination guns) can facilitate for mechanical transmission of LSD virus.
3. Diagnosis
3.1. Clinical Diagnosis
Severe cases of LSD are highly characteristic and easy to recognize and, in such cases, a clinical diagnosis can be made based on the signs and symptoms mentioned above.
The following diseases/conditions should be considered for differential diagnosis of LSD3:
- Pseudo lumpy skin disease/Bovine herpes mammillitis (bovine herpes virus 2): dermal lesions may look like those caused by LSD virus, but are more superficial as lesions involve only the epidermis. Generally, the course of disease is shorter and less severe.
- Insect bites, urticaria, and photosensitisation: dermal lesions may look like those caused by LSD virus, but are more superficial and the course of the disease is shorter and less severe.
- Pseudocowpox (Parapoxvirus): lesions occur only on the teats and udder.
- Dermatophytosis: ringworm lesions are more superficial, not usually raised and ulcerative.
- Demodicosis: dermal lesions predominantly occur over the withers, neck, back, and flanks, often with alopecia present. The disease can be ruled out by detection of mites using skin scrapings.
- Bovine papular stomatitis (Parapoxvirus): lesions occur only in the mucous membranes of the mouth.
- Besnoitiosis: lesions often occur in scleral conjunctiva; dermal lesions may exhibit alopecia with thick and wrinkled skin.
- Onchocerciasis: dermal lesions occur most often at ventral midline. Tentative differential diagnosis can be made on the basis of clinical findings, however, confirmatory diagnosis can be accomplished via PCR testing.
3.2. Laboratory diagnosis
Early stages of infection and mild cases may be difficult to diagnose clinically even for the most experienced veterinarians, hence, a laboratory confirmation is required. Samples should be collected from suspected animals and shipped to a laboratory (see Section 4) for confirmatory diagnosis by PCR assay.
Once the presence of LSD virus in a geographic region is confirmed, the subsequent diagnosis is usually based on clinical findings. However, suspected cases in a new location might require confirmatory laboratory diagnosis. Samples should be collected from all the suspected animals or at least five animals when herd size is large. Samples collected from animals should be considered infectious and standard personal protective equipment (gown, mask and hand gloves) should be used. A sufficient amount of appropriate sampling equipment required for the targeted sample types should be prepared well ahead. Precautions should be taken to avoid possible cross- contamination. All samples must be properly and permanently labeled with a unique indentation number. The collected samples should be transported to the Central Disease Investigation Laboratory (CDIL) of DLS. Contact the laboratory before shipment of the samples and inform them that the samples may contain potentially infectious LSD virus. Gel-based and real-time PCR protocols are available for the diagnosis of capripox viruses.
3.2.1. Preferred sample types
- Scabs or full-thickness skin biopsy with lesions is the preferred sample for the detection of LSD virus by PCR.
- At the early stage of infection, full blood samples with EDTA (4-12 days post- infection) and saliva or nasal swabs (12 – 18 days post-infection) also may be collected for the detection of LSD virus by PCR.
- Serum samples are of little diagnostic use as the antibodies developed following infection, vaccination or any previous exposure cannot be differentiated.
3.2.2. Sample collection and preservation
- Scabs are excellent sample material as they are easy to collect, do not require sedation of the animal or local anaesthesia, and contain high concentrations of viruses that survive long transport well in different temperatures.
A pooled sample from three different sites on an animal should be collected.
- A full-thickness skin biopsy can be collected surgically following sedation and local anesthesia. Disposable biopsy punches of around 15 mm diameter can be used.
- Saliva or nasal swabs can be collected using sterile swabs.
- Full blood samples in EDTA should be collected from the jugular or tail (coccygeal) vein. Approximately 4 ml of blood should be collected in an EDTA tube or EDTA vacutainer (purple top).
- Blood for serum samples must be collected without anticoagulant. After collection, tubes should be allowed to stand at ambient temperature for at least 1-2 hours in an upright position to let the clot begin to contract. The clot can then be loosened using a sterile rod and tubes stored at 4 °C for 12 hours. The serum can be removed with a pipette or decanted into fresh tubes. If it is necessary to clear the serum, the samples can be centrifuged at a slow speed (1000 g/2000 rmp) for 15 minutes, after which serum can be removed.
Tissue samples should be collected aseptically using sterile instruments and placed in sterile screw-capped tubes. Swabs should be placed in screw-capped tubes containing a virus transport medium (VTM). Serum samples should also be collected in screw- capped tubes. Collected samples should be kept at 2 – 6 °C if the samples can be shipped to the laboratory within 48 hours. Otherwise, the samples should be stored frozen at – 20 °C.
3.2.3. Sample transportation
- The recipient laboratory must be contacted prior to the shipment of the sample.
- It is essential that the right samples are selected, carefully labeled, packaged, and sent to the laboratory at the right temperature using the fastest practical means of transport by the most direct route.
Samples must be accompanied by a laboratory submission form (Annexure-01).
4. Disease management
4.1 Isolation, hygiene, biosecurity and insect control
- Suspected case(s) should be isolated from the rest of the herd and kept under a mosquito net.
- The rest of the animals (in-contact animals in the affected herd) should be isolated from neighbouring herd(s) for at least two weeks by avoiding communal grazing, feeding and watering.
- Clinical examinations and/or close observations should be carried out on the rest of the animals in the affected herd. Results should be systematically recorded, including rectal temperature whenever possible, in order to determine if any of the animals may already be incubating the disease.
- Neighbouring farmers, and those who have bought or sold animals from/to the affected farm recently, should be notified and placed under intensified surveillance.
- Cattle movement to and from the farm should be halted and visitors limited to essential services.
- Use of mosquito net may be considered wherever practical.
- Manure should be removed quickly and stored at a distance from the shed. Equipment used for manure removed should be cleaned and disinfected.
- Bushes and other insect habitats should be removed from the farm premises and surrounding area.
- Farm drainage systems must be cleaned as much as possible and an insecticide (mosquitocide) applied to control mosquito breeding.
- Farm sheds and the farm premises must be reguarly cleaned and disinfected. Phenol (2%), sodium hypochlorite (2–3%), iodine compounds (1:33), Virkon® (2%) and quaternary ammonium compounds (0.5%) can be used as disinfectants4.
- New needles should be used for inoculating each animal. If it is necessary to use a single needle for multiple animals, the needle should be disinfected with 70% alcohol before use in each animal.
- Awareness should be raised among the farmers, animal attendants, milkmen and artificial inseminators.
4.2 Treatment of the affected animals
There is no specific treatment for LSD. Animals with a mild infection having no fever may not need any treatment at all. Palliative and supportive care and prevention of secondary bacterial infections may be needed for severely affected animals to speed up their general recovery and promote healing of the exposed skin and mouth lesions.
In case of mild infection (a few nodules on the skin), the following treatment can be provided:
- Antipyretics (if there is fever)
- Antihistamines
- Immunity enhancers including zinc and vitamin C
In the case of systemic complications or comorbidities, the following treatment can be provided:
- Open ulcerative skin lesions should be treated with topical wound spray (bacteriocidal or bacteriostatic) twice a day with dressing. This will prevent bacterial infection and myaisis.
- Non-steroidal anti-inflammatory drugs (NSAIDs) can be used to decrease fever and pain.
- Antihistamines, electrolytes, and immunity enhancers can be used.
- Antibiotics may be needed for treatment of pneumonia or mastitis. Note: The promotion of antimicrobial resistance should be considered before prescribing any antibiotics and the reserved group of antibiotics are not recommended (https://adoptaware.org/).
- In case of severely affected calves, a bronchodilator with corticosteroids (e.g., prednisolone/dexamethasone) along with the above treatments can be provided.
5. Vaccination
LSD can be protected by prophylactic vaccination. Currently only live attenuated vaccines are available, which are based on either attenuated LSD or goat pox viruses. A vaccine based on the Gorgan strain of the goat pox virus has been found to be equally effective as the vaccine based on the Neethling strain of the LSD virus in preventing infection (5). Both types of vaccines are commercially available in Bangladesh. The goat pox vaccine is produced at the Livestock Research Institute of DLS and is being used against LSD as an emergency response. Manufacturer’s instructions should be followed for vaccinating animals.
Details for vaccination against LSD are further discussed in the DLS vaccination strategy.
6. References
- OIE (2019). Terrestrial Animal Health Code. Chapter 11.9. Infection with lumpy skin disease virus. Available at: https://www.oie.int/en/what-we-do/standards/codes-and- manuals/terrestrial-code-online-access/?id=169&L=1&htmfile=chapitre_lsd.htm
- OIE (2019). Manual of Diagnostic Tests and Vaccines for Terrestrial Animals. Chapter 3.4.12. Lumpy Skin Disease. Available at: https://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/3.04.12_LSD.pdf
- Tuppurainen, E., Alexandrov, T. & Beltrán-Alcrudo, D. (2017). Lumpy skin disease – A field manual for veterinarians. FAO Animal Production and Health Manual No. 20. Rome. Food and Agriculture Organization of the United Nations (FAO). 60 pp. Available at: http://www.fao.org/3/i7330en/I7330EN.pdf
- Babiuk S. (2018) Persistence and Stability of the Virus. In: Lumpy Skin Disease. Springer, Cham. https://doi.org/10.1007/978-3-319-92411-3_11
- Zhugunissova, K.; Bulatov, Y.; Orynbayev, M.; Kutumbetov, L.; Abduraimov, Y.; Shayakhmetova, Y.; Taranov, D.; Amanova, Z.; Mambetaliyev, M.; Absatova, Z.; et al. Goatpox virus (G20-LKV) vaccine strain elicits a protective response in cattle against lumpy skin disease at challenge with lumpy skin disease virulent field strain in a comparative study. Vet. Microbial. 2020, 245, 108695.
- www.dls.gov.bd


0 responses to “Guidelines for Clinical Management of Lumpy Skin Disease in Bangladesh”